
As of May 11, 2020, there are 67,152 confirmed cases of COVID-19 in India. Since May 4, 24,619 new cases have been registered. Out of the confirmed cases so far, 20,917 patients have been cured/discharged and 2,206 have died. As the spread of COVID-19 has increased across the country, the central government has continued to announce several policy decisions to contain the spread, and support citizens and businesses who are being affected by the pandemic. In this blog post, we summarise some of the key measures taken by the central government in this regard between May 4 and May 11, 2020.
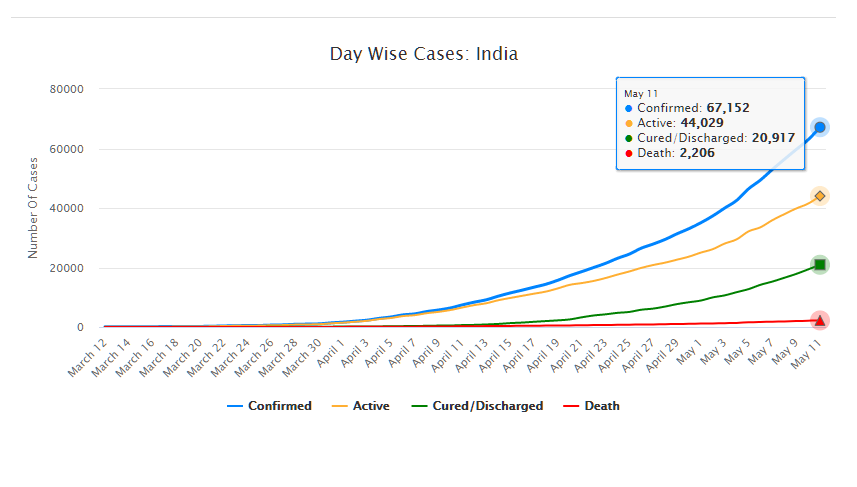
Source: Ministry of Health and Family Welfare; PRS.
Industry
Relaxation of labour laws in some states
The Gujarat, Himachal Pradesh, Rajasthan, Haryana, and Uttarakhand governments have passed notifications to increase maximum weekly work hours from 48 hours to 72 hours and daily work hours from 9 hours to 12 hours for certain factories. This was done to combat the shortage of labour caused by the lockdown. Further, some state governments stated that longer shifts would ensure a fewer number of workers in factories so as to allow for social distancing.
Madhya Pradesh has promulgated the Madhya Pradesh Labour Laws (Amendment) Ordinance, 2020. The Ordinance exempts establishments with less than 100 workers from adhering to the Madhya Pradesh Industrial Employment (Standing Orders) Act, 1961, which regulates the conditions of employment of workers. Further, it allows the state government to exempt any establishment or class of establishments from the Madhya Pradesh Shram Kalyan Nidhi Adhiniyam, 1982, which provides for the constitution of a welfare fund for labour.
The Uttar Pradesh government has published a draft Ordinance which exempts all factories and establishments engaged in manufacturing processes from all labour laws for a period of three years. Certain conditions will continue to apply with regard to payment of wages, safety, compensation and work hours, amongst others. However, labour laws providing for social security, industrial dispute resolution, trade unions, strikes, amongst others, will not apply under the Ordinance.
Financial aid
Central government signs an agreement with Asian Infrastructure Investment Bank for COVID-19 support
The central government and Asian Infrastructure Investment Bank (AIIB) signed a 500 million dollar agreement for the COVID-19 Emergency Response and Health Systems Preparedness Project. The project aims to help India respond to the COVID-19 pandemic and strengthen India’s public health system to manage future disease outbreaks. The project is being financed by the World Bank and AIIB in the amount of 1.5 billion dollars, of which one billion dollars is being provided by World Bank and 500 million dollars is being provided by AIIB. This financial support will be available to all states and union territories and will be used to address the needs of at-risk populations, medical personnel, and creating medical and testing facilities, amongst others. The project will be implemented by the National Health Mission, the National Center for Disease Control, and the Indian Council of Medical Research, under the Ministry of Health and Family Welfare.
Travel
Restarting of passenger travel by railways
Indian Railways plans to restart passenger trains from May 12 onwards. It will begin with 15 pairs of trains which will run from New Delhi station connecting Dibrugarh, Agartala, Howrah, Patna, Bilaspur, Ranchi, Bhubaneswar, Secunderabad, Bengaluru, Chennai, Thiruvananthapuram, Madgaon, Mumbai Central, Ahmedabad and Jammu Tawi. Booking for reservation in these trains will start at 4 pm on May 11. Thereafter, Indian Railways plans to start more services on new routes.
Return of Indians stranded abroad
The central government will facilitate the return of Indian nationals stranded abroad in a phased manner beginning on May 7. The travel will be arranged by aircraft and naval ships. The stranded Indians utilising the service will be required to pay for it. Medical screening of the passengers will be done before the flight. On reaching India, passengers will be required to download the Aarogya Setu app. Further, they will be quarantined by the concerned state government in either a hospital or a quarantine institution for 14 days on a payment basis. After quarantine, passengers will be tested for COVID-19 and further action will be taken based on the results.
For more information on the spread of COVID-19 and the central and state government response to the pandemic, please see here.
Recently, the Standing Committee on Health and Family Welfare submitted its report to the Parliament on the National Commission for Human Resource for Health Bill, 2011. The objective of the Bill is to “ensure adequate availability of human resources in the health sector in all states”. It seeks to set up the National Commission for Human Resources for Health (NCHRH), National Board for Health Education (NBHE), and the National Evaluation and Assessment Council (NEAC) in order to determine and regulate standards of health education in the country. It separates regulation of the education sector from that of professions such as law, medicine and nursing, and establishes professional councils at the national and state levels to regulate the professions. See here for PRS Bill Summary. The Standing Committee recommended that this Bill be withdrawn and a revised Bill be introduced in Parliament after consulting stakeholders. It felt that concerns of the professional councils such as the Medical Council of India and the Dental Council of India were not adequately addressed. Also, it noted that the powers and functions of the NCHRH and the National Commission on Higher Education and Research (to be established under the Higher Education and Research Bill, 2011 to regulate the higher education sector in the country) were overlapping in many areas. Finally, it also expressed concern over the acute shortage of qualified health workers in the country as well as variations among states and rural and urban areas. As per the 2001 Census, the estimated density of all health workers (qualified and unqualified) is about 20% less than the World Health Organisation’s norm of 2.5 health workers per 1000 population. See here for PRS Standing Committee Summary. Shortfall of health workers in rural areas Public health care in rural areas is provided through a multi-tier network. At the lowest level, there are sub health-centres for every population of 5,000 in the plains and 3,000 in hilly areas. The next level consists of Primary Health Centres (PHCs) for every population of 30,000 in the plains and 20,000 in the hills. Generally, each PHC caters to a cluster of Gram Panchayats. PHCs are required to have one medical officer and 14 other staff, including one Auxiliary Nurse Midwife (ANM). There are Community Health Centres (CHCs) for every population of 1,20,000 in the plains and 80,000 in hilly areas. These sub health centres, PHCs and CHCs are linked to district hospitals. As on March 2011, there are 14,8124 sub health centres, 23,887 PHCs and 4809 CHCs in the country.[i] Sub-Health Centres and Primary Health Centres
Table 1: State-wise comparison of vacancy in PHCs
|
Doctors at PHCs |
ANM at PHCs and Sub-Centres |
|||||
| State | Sanctioned post | Vacancy | % of vacancy | Sanctioned post | Vacancy | % of vacancy |
| Chhattisgarh | 1482 | 1058 | 71 | 6394 | 964 | 15 |
| West Bengal | 1807 | 801 | 44 | 10,356 | NA | 0 |
| Maharashtra | 3618 | 1326 | 37 | 21,122 | 0 | 0 |
| Uttar Pradesh | 4509 | 1648 | 36 | 25,190 | 2726 | 11 |
| Mizoram | 57 | 20 | 35 | 388 | 0 | 0 |
| Madhya Pradesh | 1238 | 424 | 34 | 11,904 | 0 | 0 |
| Gujarat | 1123 | 345 | 31 | 7248 | 817 | 11 |
| Andaman & Nicobar Isld | 40 | 12 | 30 | 214 | 0 | 0 |
| Odisha | 725 | 200 | 28 | 7442 | 0 | 0 |
| Tamil Nadu | 2326 | 622 | 27 | 9910 | 136 | 1 |
| Himachal Pradesh | 582 | 131 | 22 | 2213 | 528 | 24 |
| Uttarakhand | 299 | 65 | 22 | 2077 | 0 | 0 |
| Manipur | 240 | 48 | 20 | 984 | 323 | 33 |
| Haryana | 651 | 121 | 19 | 5420 | 386 | 7 |
| Sikkim | 48 | 9 | 19 | 219 | 0 | 0 |
| Meghalaya | 127 | 23 | 18 | 667 | 0 | 0 |
| Delhi | 22 | 3 | 14 | 43 | 0 | 0 |
| Goa | 46 | 5 | 11 | 260 | 20 | 8 |
| Karnataka | 2310 | 221 | 10 | 11,180 | 0 | 0 |
| Kerala | 1204 | 82 | 7 | 4232 | 59 | 1 |
| Andhra Pradesh | 2424 | 76 | 3 | 24,523 | 2876 | 12 |
| Rajasthan | 1478 | 6 | 0.4 | 14,348 | 0 | 0 |
| Arunachal Pradesh | NA | NA | NA | NA | NA | 0 |
| Assam | NA | NA | NA | NA | NA | 0 |
| Bihar | 2078 | 0 | NA | NA | NA | 0 |
| Chandigarh | 0 | 0 | NA | 17 | 0 | 0 |
| Dadra & Nagar Haveli | 6 | 0 | NA | 40 | 0 | 0 |
| Daman & Diu | 3 | 0 | NA | 26 | 0 | 0 |
| Jammu & Kashmir | 750 | 0 | NA | 2282 | 0 | 0 |
| Jharkhand | 330 | 0 | NA | 4288 | 0 | 0 |
| Lakshadweep | 4 | 0 | NA | NA | NA | 0 |
| Nagaland | NA | NA | NA | NA | NA | 0 |
| Puducherry | 37 | 0 | NA | 72 | 0 | 0 |
| Punjab | 487 | 0 | NA | 4044 | 0 | 0 |
| Tripura | NA | NA | NA | NA | NA | 0 |
| India | 30,051 | 7,246 | 24 | 1,77,103 | 8,835 | 5 |
| Sources: National Rural Health Mission (available here), PRS.Note: The data for all states is as of March 2011 except for some states where data is as of 2010. For doctors, these states are Bihar, UP, Mizoram and Delhi. For ANMs, these states are Odisha and Uttar Pradesh. | ||||||
Community Health Centres
Table 2: Vacancies in CHCs of medical specialists
| Surgeons | Gynaecologists | Physicians | Paediatricians | |
| State |
% of vacancy |
|||
| Andaman & NicobarIsland | 100 | 100 | 100 | 100 |
| Andhra Pradesh | 74 | 0 | 45 | 3 |
| Arunachal Pradesh | NA | NA | NA | NA |
| Assam | NA | NA | NA | NA |
| Bihar | 41 | 44 | 60 | 38 |
| Chandigarh | 50 | 40 | 50 | 100 |
| Chhattisgarh | 85 | 85 | 90 | 84 |
| Dadra & Nagar Haveli | 0 | 0 | 0 | 0 |
| Daman & Diu | 0 | 100 | 0 | 100 |
| Delhi | 0 | 0 | 0 | 0 |
| Goa | 20 | 20 | 67 | 66 |
| Gujarat | 77 | 73 | 0 | 91 |
| Haryana | 71 | 80 | 94 | 85 |
| Himachal Pradesh | NA | NA | NA | NA |
| Jammu & Kashmir | 34 | 34 | 53 | 63 |
| Jharkhand | 45 | 0 | 81 | 61 |
| Karnataka | 33 | NA | NA | NA |
| Kerala | NA | NA | NA | NA |
| Lakshadweep | 0 | 0 | 100 | 0 |
| Madhya Pradesh | 78 | 69 | 76 | 58 |
| Maharashtra | 21 | 0 | 34 | 0 |
| Manipur | 100 | 94 | 94 | 87 |
| Meghalaya | 50 | NA | 100 | 50 |
| Mizoram | NA | NA | NA | NA |
| Nagaland | NA | NA | NA | NA |
| Odisha | 44 | 45 | 62 | 41 |
| Puducherry | 0 | 0 | 100 | NA |
| Punjab | 16 | 36 | 40 | 48 |
| Rajasthan | 57% | 46 | 49 | 24 |
| Sikkim | NA | NA | NA | NA |
| Tamil Nadu | 0 | 0 | 0 | 0 |
| Tripura | NA | NA | NA | NA |
| Uttar Pradesh | NA | NA | NA | NA |
| Uttarakhand | 69 | 63 | 74 | 40 |
| West Bengal | 0 | 57 | 0 | 78 |
| India | 56 | 47 | 59 | 49 |
| Sources: National Rural Health Mission (available here), PRS. | ||||
[i]. “Rural Healthcare System in India”, National Rural Health Mission (available here).