
The National Medical Commission (NMC) Bill, 2017 was introduced in Lok Sabha in December, 2017. It was examined by the Standing Committee on Health, which submitted its report during Budget Session 2018. The Bill seeks to regulate medical education and practice in India. In this post, we analyse the Bill in its current form.
How is medical education and practice regulated currently?
The Medical Council of India (MCI) is responsible for regulating medical education and practice. Over the years, there have been several issues with the functioning of the MCI with respect to its regulatory role, composition, allegations of corruption, and lack of accountability. For example, MCI is an elected body where its members are elected by medical practitioners themselves, i.e. the regulator is elected by the regulated. In light of such issues, experts recommended nomination based constitution of the MCI instead of election, and separating the regulation of medical education and medical practice. They suggested that legislative changes should be brought in to overhaul the functioning of the MCI.
To meet this objective, the Bill repeals the Indian Medical Council Act, 1956 and dissolves the current Medical Council of India (MCI) which regulates medical education and practice.
Who will be a part of the NMC?
The NMC will consist of 25 members, of which at least 17 (68%) will be medical practitioners. The Standing Committee has noted that the current MCI is non-diverse and consists mostly of doctors who look out for their own self-interest over larger public interest. In order to reduce the monopoly of doctors, it recommended that the MCI should include diverse stakeholders such as public health experts, social scientists, and health economists. In other countries, such as the United Kingdom, the General Medical Council (GMC) responsible for regulating medical education and practice consists of 12 medical practitioners and 12 lay members (such as community health members, and administrators from the local government).
How will the issues of medical misconduct be addressed?
The State Medical Council will receive complaints relating to professional or ethical misconduct against a registered doctor. If the doctor is aggrieved by the decision of the State Medical Council, he may appeal to the Ethics and Medical Registration Board, and further before the NMC. Appeals against the decision of the NMC will lie before the central government. It is unclear why the central government is an appellate authority with regard to such matters.
It may be argued that disputes related to ethics and misconduct in medical practice may require judicial expertise. For example, in the UK, the GMC receives complaints with regard to ethical misconduct and is required to do an initial documentary investigation. It then forwards the complaint to a Tribunal, which is a judicial body independent of the GMC. The adjudication and final disciplinary action is decided by the Tribunal.
What will the NMC’s role be in fee regulation of private medical colleges?
In India, the Supreme Court has held that private providers of education have to operate as charitable and not for profit institutions. Despite this, many private education institutions continue to charge exorbitant fees which makes medical education unaffordable and inaccessible to meritorious students. Currently, for private unaided medical colleges, the fee structure is decided by a committee set up by state governments under the chairmanship of a retired High Court judge. The Bill allows the NMC to frame guidelines for determination of fees for up to 40% of seats in private medical colleges and deemed universities. The question is whether the NMC as a regulator should regulate fees charged by private medical colleges.
A NITI Aayog Committee (2016) was of the opinion that a fee cap would discourage the entry of private colleges, therefore, limiting the expansion of medical education. It also observed that it is difficult to enforce such a fee cap and could lead medical colleges to continue charging high fees under other pretexts.
Note that the Parliamentary Standing Committee (2018) which examined the Bill has recommended continuing the current system of fee structures being decided by the Committee under the chairmanship of a retired High Court judge. However, for those private medical colleges and deemed universities, unregulated under the existing mechanism, fee must be regulated for at least 50% of the seats. The Union Cabinet has approved an Amendment to increase the regulation of fees to 50% of seats.
How will doctors become eligible to practice?
The Bill introduces a National Licentiate Examination for students graduating from medical institutions in order to obtain a licence to practice as a medical professional.
However, the NMC may permit a medical practitioner to perform surgery or practice medicine without qualifying the National Licentiate Examination, in such circumstances and for such period as may be specified by regulations. The Ministry of Health and Family Welfare has clarified that this exemption is not meant to allow doctors failing the National Licentiate Examination to practice but is intended to allow medical professionals like nurse practitioners and dentists to practice. It is unclear from the Bill that the term ‘medical practitioner’ includes medical professionals (like nurses) other than MBBS doctors.
Further, the Bill does not specify the validity period of this licence to practice. In other countries such as the United Kingdom and Australia, a licence to practice needs to be periodically renewed. For example, in the UK the licence has to be renewed every five years, and in Australia it has to renewed annually.
What are the issues around the bridge course for AYUSH practitioners to prescribe modern medicine?
The debate around AYUSH practitioners prescribing modern medicine
There is a provision in the Bill which states that there may be a bridge course which AYUSH practitioners (practicing Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy) can undertake in order to prescribe certain kinds of modern medicine. There are differing views on whether AYUSH practitioners should prescribe modern medicines.
Over the years, various committees have recommended a functional integration among various systems of medicine i.e. Ayurveda, modern medicine, and others. On the other hand, experts state that the bridge course may promote the positioning of AYUSH practitioners as stand-ins for allopathic doctors owing to the shortage of doctors across the country. This in turn may affect the development of AYUSH systems of medicine as independent systems of medicine.
Moreover, AYUSH doctors do not have to go through any licentiate examination to be registered by the NMC, unlike the other doctors. Recently, the Union Cabinet has approved an Amendment to remove the provision of the bridge course.
Status of other kinds of medical personnel
As of January 2018, the doctor to population ratio in India was 1:1655 compared to the World Health Organisation standard of 1:1000. The Ministry of Health and Family Welfare stated that the introduction of the bridge course for AYUSH practitioners under the Bill will help fill in the gaps of availability of medical professionals.
If the purpose of the bridge course is to address shortage of medical professionals, it is unclear why the option to take the bridge course does not apply to other cadres of allopathic medical professionals such as nurses, and dentists. There are other countries where medical professionals other than doctors are allowed to prescribe allopathic medicine. For example, Nurse Practitioners in the USA provide a full range of primary, acute, and specialty health care services, including ordering and performing diagnostic tests, and prescribing medications. For this purpose, Nurse Practitioners must complete a master’s or doctoral degree program, advanced clinical training, and obtain a national certification.
As of May 11, 2020, there are 67,152 confirmed cases of COVID-19 in India. Since May 4, 24,619 new cases have been registered. Out of the confirmed cases so far, 20,917 patients have been cured/discharged and 2,206 have died. As the spread of COVID-19 has increased across the country, the central government has continued to announce several policy decisions to contain the spread, and support citizens and businesses who are being affected by the pandemic. In this blog post, we summarise some of the key measures taken by the central government in this regard between May 4 and May 11, 2020.
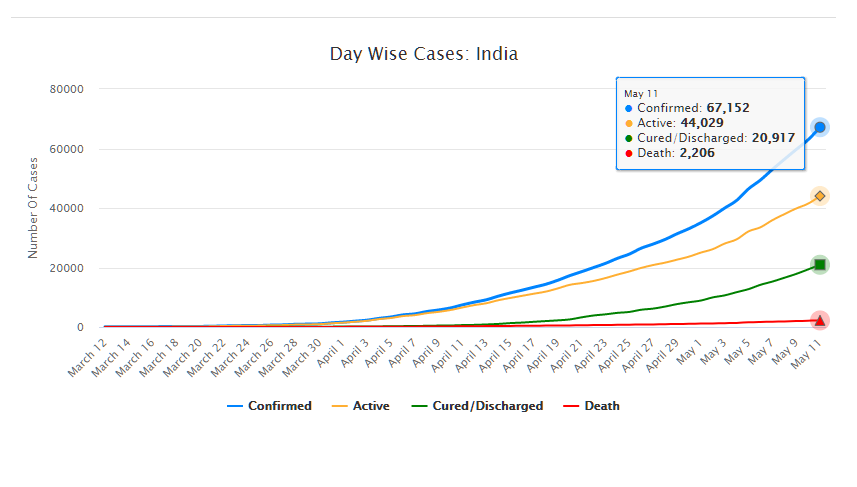
Source: Ministry of Health and Family Welfare; PRS.
Industry
Relaxation of labour laws in some states
The Gujarat, Himachal Pradesh, Rajasthan, Haryana, and Uttarakhand governments have passed notifications to increase maximum weekly work hours from 48 hours to 72 hours and daily work hours from 9 hours to 12 hours for certain factories. This was done to combat the shortage of labour caused by the lockdown. Further, some state governments stated that longer shifts would ensure a fewer number of workers in factories so as to allow for social distancing.
Madhya Pradesh has promulgated the Madhya Pradesh Labour Laws (Amendment) Ordinance, 2020. The Ordinance exempts establishments with less than 100 workers from adhering to the Madhya Pradesh Industrial Employment (Standing Orders) Act, 1961, which regulates the conditions of employment of workers. Further, it allows the state government to exempt any establishment or class of establishments from the Madhya Pradesh Shram Kalyan Nidhi Adhiniyam, 1982, which provides for the constitution of a welfare fund for labour.
The Uttar Pradesh government has published a draft Ordinance which exempts all factories and establishments engaged in manufacturing processes from all labour laws for a period of three years. Certain conditions will continue to apply with regard to payment of wages, safety, compensation and work hours, amongst others. However, labour laws providing for social security, industrial dispute resolution, trade unions, strikes, amongst others, will not apply under the Ordinance.
Financial aid
Central government signs an agreement with Asian Infrastructure Investment Bank for COVID-19 support
The central government and Asian Infrastructure Investment Bank (AIIB) signed a 500 million dollar agreement for the COVID-19 Emergency Response and Health Systems Preparedness Project. The project aims to help India respond to the COVID-19 pandemic and strengthen India’s public health system to manage future disease outbreaks. The project is being financed by the World Bank and AIIB in the amount of 1.5 billion dollars, of which one billion dollars is being provided by World Bank and 500 million dollars is being provided by AIIB. This financial support will be available to all states and union territories and will be used to address the needs of at-risk populations, medical personnel, and creating medical and testing facilities, amongst others. The project will be implemented by the National Health Mission, the National Center for Disease Control, and the Indian Council of Medical Research, under the Ministry of Health and Family Welfare.
Travel
Restarting of passenger travel by railways
Indian Railways plans to restart passenger trains from May 12 onwards. It will begin with 15 pairs of trains which will run from New Delhi station connecting Dibrugarh, Agartala, Howrah, Patna, Bilaspur, Ranchi, Bhubaneswar, Secunderabad, Bengaluru, Chennai, Thiruvananthapuram, Madgaon, Mumbai Central, Ahmedabad and Jammu Tawi. Booking for reservation in these trains will start at 4 pm on May 11. Thereafter, Indian Railways plans to start more services on new routes.
Return of Indians stranded abroad
The central government will facilitate the return of Indian nationals stranded abroad in a phased manner beginning on May 7. The travel will be arranged by aircraft and naval ships. The stranded Indians utilising the service will be required to pay for it. Medical screening of the passengers will be done before the flight. On reaching India, passengers will be required to download the Aarogya Setu app. Further, they will be quarantined by the concerned state government in either a hospital or a quarantine institution for 14 days on a payment basis. After quarantine, passengers will be tested for COVID-19 and further action will be taken based on the results.
For more information on the spread of COVID-19 and the central and state government response to the pandemic, please see here.