
The Medical Council of India (MCI) has seen a few major controversies over the past decade. In the latest incident, MCI President, Dr. Ketan Desai was arrested by the CBI on charges of accepting a bribe for granting recognition to Gyan Sagar Medical College in Punjab. Following this incident, the central government promulgated an ordinance dissolving the MCI and replacing it with a centrally nominated seven member board. The ordinance requires MCI to be re-constituted within one year of its dissolution in accordance with the provisions of the original Act. Background The Medical Council of India was first established in 1934 under the Indian Medical Council Act, 1933. This Act was repealed and replaced with a new Act in 1956. Under the 1956 Act, the objectives of MCI include:
Over the years, several committees, the most recent being the National Knowledge Commission (NKC) and the Yashpal Committee, have commented on the need for reforms in medical regulation in the country. The Ministry of Health and Family Welfare (MoH&FW) has recently released a draft of the National Council for Human Resources in Health (NCHRH) Bill for public feedback. (See http://mohfw.nic.in/nchrc-health.htm) Key issues in Medical Regulation Oversight Currently, separate regulatory bodies oversee the different healthcare disciplines. These include the Medical Council of India, the Indian Nursing Council, the Dental Council of India, the Rehabilitation Council of India and the Pharmacy Council of India. Each Council regulates both education and professional practice within its domain. The draft NCHRH Bill proposes to create an overarching body to subsume these councils into a single structure. This new body, christened the National Council for Human Resources in Health (NCHRH) is expected to encourage cross connectivity across these different health-care disciplines. Role of Councils Both the NKC and the Yashpal Committee make a case for separating regulation of medical education from that of profession. It is recommended that the current councils be divested of their education responsibilities and that these work solely towards regulation of professionals – prescribing a code of ethics, ensuring compliance, and facilitating continued medical education. In addition, it has been recommended that a national exit level examination be conducted. This exit examination should then serve the purpose of ‘occupational licensing’, unlike the prevalent registration system that automatically grants practice rights to graduating professionals. In effect, it is envisaged that the system be reconfigured on the lines of the Institute of Chartered Accountants, wherein the council restricts itself to regulating the profession, but has an indirect say in education through its requirements on the exit examination. A common national examination is also expected to ensure uniformity in quality across the country. Both committees also recommend enlisting independent accrediting agencies for periodically evaluating medical colleges on pre-defined criteria and making this information available to the public (including students). This is expected to bring more transparency into the system. Supervision of education – HRD vs. H&FW The Ministry of Human Resources and Development (MHRD) is proposing a National Council for Higher Education and Research (NCHER) to regulate all university education. However, MoH&FW is of the opinion that Medical Education is a specialized field and needs focused attention, and hence should be regulated separately. However, it is worth noting that both the NKC and the Yashpal Committee recommend transferring education overseeing responsibilities to the NCHER. Internationally, different models exist across countries. In the US, the Higher Education Act, 1965 had transferred all education responsibilities to the Department of Education. In the UK, both medical education and profession continue to be regulated by the General Medical Council (the MCI counterpart), which is different from the regulator for Higher Education. Composition of Councils In 2007-08, MCI, when fully constituted, was a 129 member body. The Ministry in its draft NCHRH Bill makes a case for reducing this size. The argument advanced is that such a large size makes the council unwieldy in character and hence constrains reform. In 2007-08, 71% of the members in the committee were elected. These represented universities and doctors registered across the country. However, the Standing Committee on H&FW report (2006) points out that delays in conducting elections usually leads to several vacancies in this category, thereby reducing the actual percentage of elected members. MCI’s 2007-08 annual report mentions that at the time of publishing the report, 29 seats (32% of elected category) were vacant due to ‘various reasons like expiry of term, non-election of a member, non-existence of medical faculty of certain Universities’. In November 2001, the Delhi High Court set aside the election of Dr. Ketan Desai as President of the MCI, stating that he had been elected under a ‘flawed constitution’. The central government had failed to ensure timely conduct of elections to the MCI. As a result, a number of seats were lying vacant. The Court ordered that the MCI be reconstituted at the earliest and appointed an administrator to oversee the functioning of the MCI until this was done. Several countries like the UK are amending their laws to make council membership more broad-based by including ‘lay-members’/ non-doctors. The General Medical Council in the UK was recently reconstituted and it now comprises of 24 members - 12 ‘lay’ and 12 medical members. (See http://www.gmc-uk.org/about/council.asp) Way ahead According to latest news reports, the MoH&FW is currently revising the draft Bill. Let's wait and see how the actual legislation shapes up. Watch this space for further updates!
As of May 11, 2020, there are 67,152 confirmed cases of COVID-19 in India. Since May 4, 24,619 new cases have been registered. Out of the confirmed cases so far, 20,917 patients have been cured/discharged and 2,206 have died. As the spread of COVID-19 has increased across the country, the central government has continued to announce several policy decisions to contain the spread, and support citizens and businesses who are being affected by the pandemic. In this blog post, we summarise some of the key measures taken by the central government in this regard between May 4 and May 11, 2020.
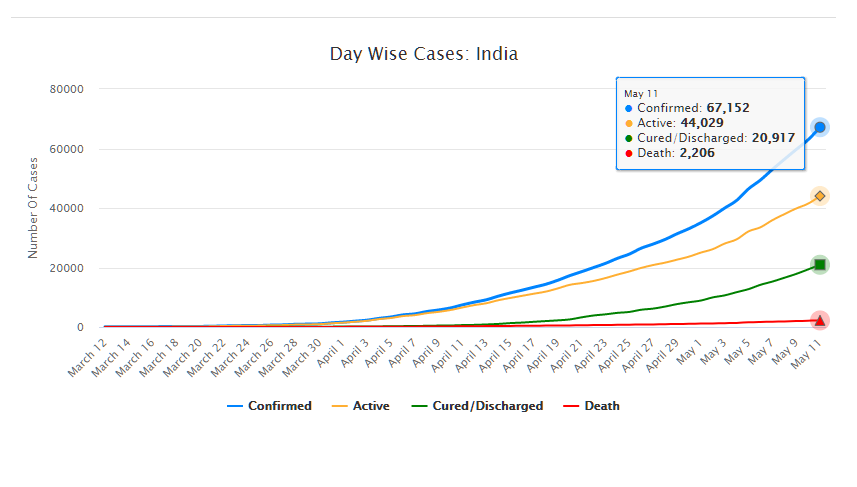
Source: Ministry of Health and Family Welfare; PRS.
Industry
Relaxation of labour laws in some states
The Gujarat, Himachal Pradesh, Rajasthan, Haryana, and Uttarakhand governments have passed notifications to increase maximum weekly work hours from 48 hours to 72 hours and daily work hours from 9 hours to 12 hours for certain factories. This was done to combat the shortage of labour caused by the lockdown. Further, some state governments stated that longer shifts would ensure a fewer number of workers in factories so as to allow for social distancing.
Madhya Pradesh has promulgated the Madhya Pradesh Labour Laws (Amendment) Ordinance, 2020. The Ordinance exempts establishments with less than 100 workers from adhering to the Madhya Pradesh Industrial Employment (Standing Orders) Act, 1961, which regulates the conditions of employment of workers. Further, it allows the state government to exempt any establishment or class of establishments from the Madhya Pradesh Shram Kalyan Nidhi Adhiniyam, 1982, which provides for the constitution of a welfare fund for labour.
The Uttar Pradesh government has published a draft Ordinance which exempts all factories and establishments engaged in manufacturing processes from all labour laws for a period of three years. Certain conditions will continue to apply with regard to payment of wages, safety, compensation and work hours, amongst others. However, labour laws providing for social security, industrial dispute resolution, trade unions, strikes, amongst others, will not apply under the Ordinance.
Financial aid
Central government signs an agreement with Asian Infrastructure Investment Bank for COVID-19 support
The central government and Asian Infrastructure Investment Bank (AIIB) signed a 500 million dollar agreement for the COVID-19 Emergency Response and Health Systems Preparedness Project. The project aims to help India respond to the COVID-19 pandemic and strengthen India’s public health system to manage future disease outbreaks. The project is being financed by the World Bank and AIIB in the amount of 1.5 billion dollars, of which one billion dollars is being provided by World Bank and 500 million dollars is being provided by AIIB. This financial support will be available to all states and union territories and will be used to address the needs of at-risk populations, medical personnel, and creating medical and testing facilities, amongst others. The project will be implemented by the National Health Mission, the National Center for Disease Control, and the Indian Council of Medical Research, under the Ministry of Health and Family Welfare.
Travel
Restarting of passenger travel by railways
Indian Railways plans to restart passenger trains from May 12 onwards. It will begin with 15 pairs of trains which will run from New Delhi station connecting Dibrugarh, Agartala, Howrah, Patna, Bilaspur, Ranchi, Bhubaneswar, Secunderabad, Bengaluru, Chennai, Thiruvananthapuram, Madgaon, Mumbai Central, Ahmedabad and Jammu Tawi. Booking for reservation in these trains will start at 4 pm on May 11. Thereafter, Indian Railways plans to start more services on new routes.
Return of Indians stranded abroad
The central government will facilitate the return of Indian nationals stranded abroad in a phased manner beginning on May 7. The travel will be arranged by aircraft and naval ships. The stranded Indians utilising the service will be required to pay for it. Medical screening of the passengers will be done before the flight. On reaching India, passengers will be required to download the Aarogya Setu app. Further, they will be quarantined by the concerned state government in either a hospital or a quarantine institution for 14 days on a payment basis. After quarantine, passengers will be tested for COVID-19 and further action will be taken based on the results.
For more information on the spread of COVID-19 and the central and state government response to the pandemic, please see here.